Epistaxis / Nose Bleeding
नकसीर / एपिस्टेक्सिस
What is Epistaxis?
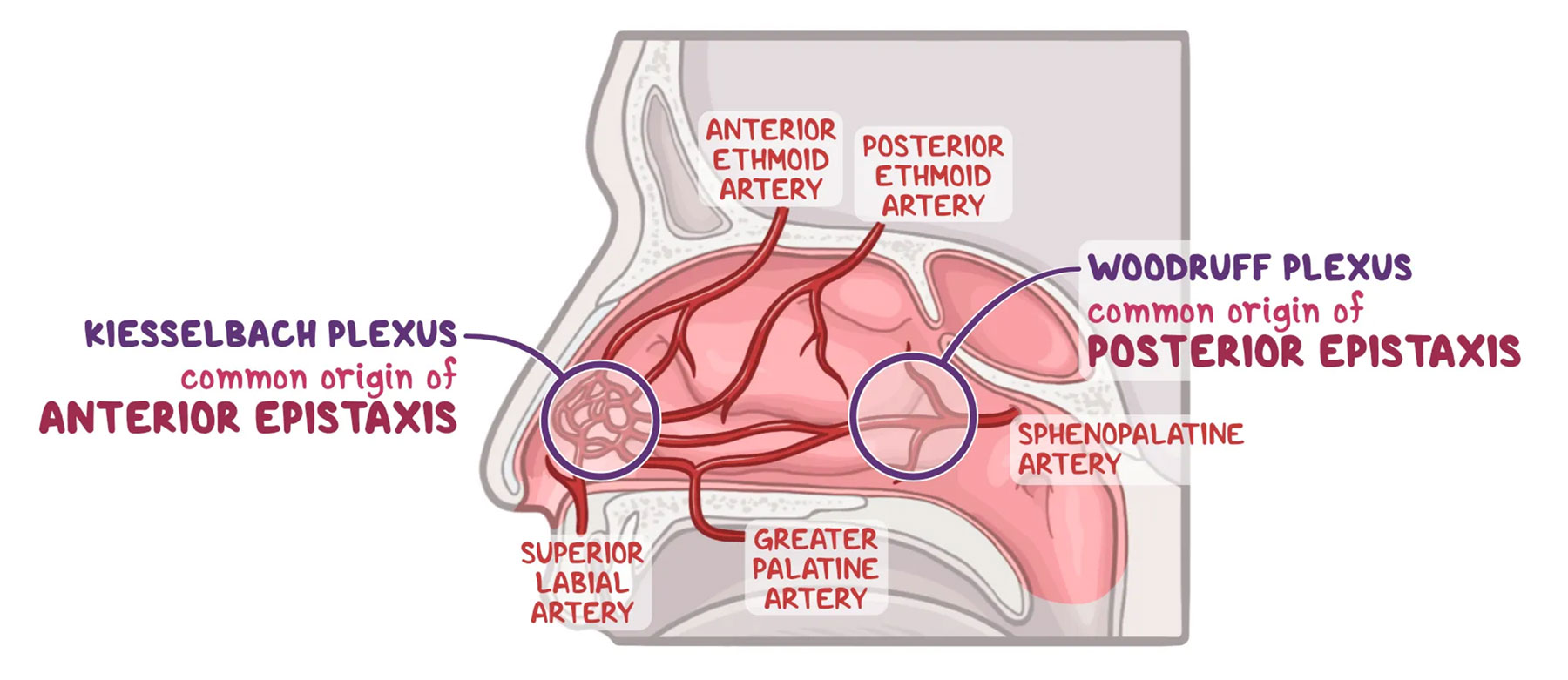
Epistaxis (also called a nosebleed) refers to a minor bleeding from the blood vessels of the nose. Epistaxis is a commonly-found complaint, especially in fields of emergency medicine related to the treatment of ear, nose, and throat (ENT) conditions. Epistaxis more commonly occurs in children (ages 2–10) and older adults (ages 50–80). There are two types of epistaxis depending on their origin:
- Anterior Epistaxis
- Posterior Epistaxis
What is Anterior Epistaxis?
Anterior epistaxis refers to a nosebleed that originates from the anterior (frontal) part of the nose. Most of the time, cases of anterior epistaxis originate from the Kiesselbach plexus, which is a vascular network found on the nasal septum, as these arteries can be easily traumatized. Anterior epistaxis is the most common type of nosebleed, and usually involves one nostril.
What is Posterior Epistaxis?
Posterior epistaxis refers to bleeding from the posterior or superior nasal cavity. Most often, it originates from the Woodruff plexus, which is a vascular network found in the lateral wall of the nasal cavity. Posterior epistaxis usually involves both nostrils. For these types of nosebleeds, the blood may also flow backwards and uncomfortably get swallowed or coughed up (hemoptysis).